Learn About Systemic Lupus Erythematosus (SLE)
What is SLE?
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease that primarily affects young women in Hong Kong, with a female-to-male ratio of approximately 7:1 to 9:1. It is most common among individuals aged 15 to 50. The estimated prevalence is about 60 cases per 100,000 people, making it relatively rare but with significant impact.
SLE can affect multiple organs, including the skin, joints, kidneys, blood, and nervous system. Symptoms vary widely—from rashes, arthritis, and oral ulcers to nephritis—and in severe cases, it can be life-threatening. The exact cause remains unclear but is believed to involve immune system dysfunction, genetic predisposition, hormonal influences, and environmental triggers.
Causes and Symptoms
What causes SLE?
Although the exact cause is not fully understood, SLE is primarily linked to immune system dysfunction. It is a chronic autoimmune condition where the immune system mistakenly attacks the body’s own cells and tissues, causing inflammation and organ damage. Key contributing factors include:
Immune imbalance:The immune system fails to distinguish between “self” and “foreign,” producing excessive antibodies that attack healthy tissues.
Genetic factors:A family history of lupus or other autoimmune diseases increases the risk.
Hormonal influences:The significantly higher prevalence in women suggests a link to female hormones such as estrogen.
Environmental triggers:Sunlight exposure, viral infections, certain medications, and stress may trigger or worsen the condition.
Emotional and lifestyle stress:Mental strain or chronic stress is believed to exacerbate disease activity.
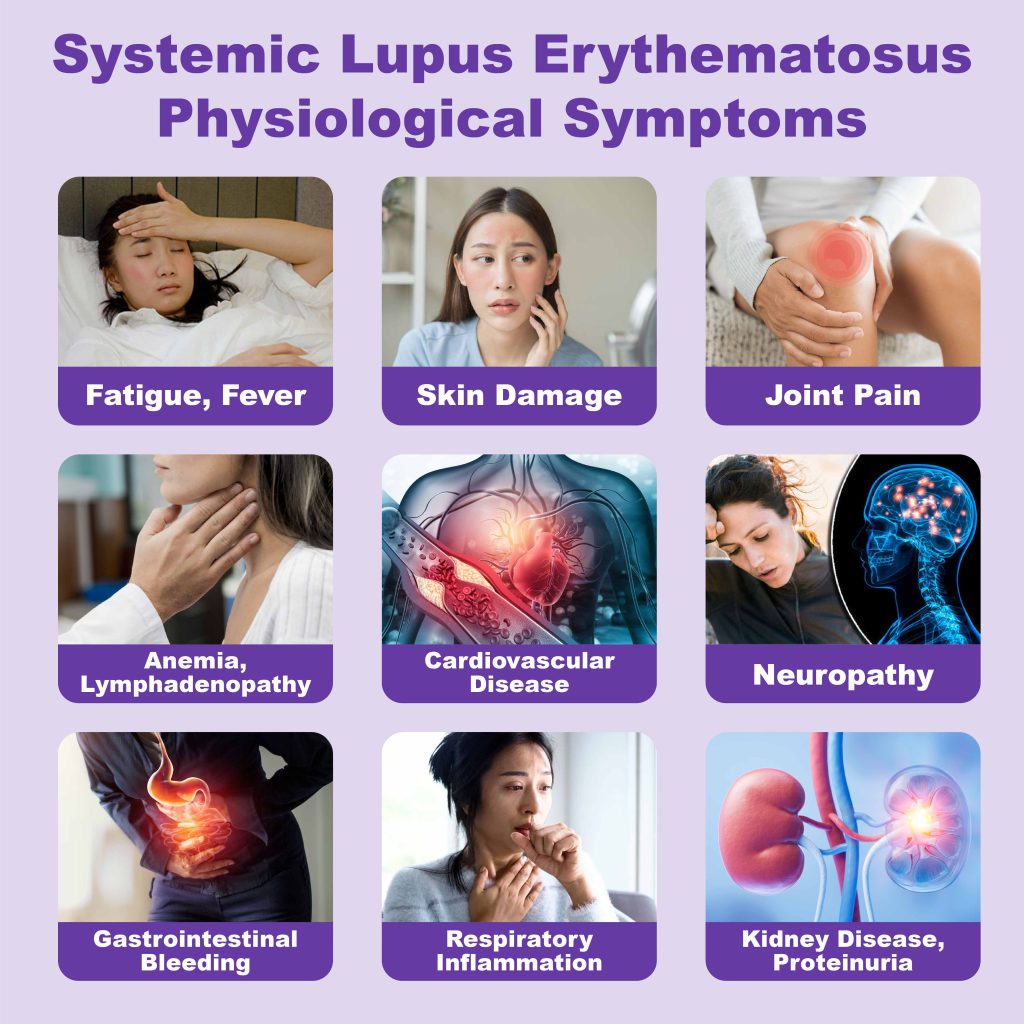
Common Symptoms of SLE
Symptoms vary from person to person and may be mild or severe. The disease often follows a pattern of flare-ups and remission.
General symptoms:Fatigue, fever, weight loss
Musculoskeletal system:Joint pain, arthritis, muscle stiffness
Skin:Classic “butterfly rash” across the nose and cheeks, discoid rash, photosensitivity, oral ulcers, hair loss
Blood system:Anemia, low white blood cell count, reduced platelets
Kidneys:Proteinuria, nephritis, nephrotic syndrome
Nervous system:Headaches, seizures, cognitive impairment, mood disorders
Cardiopulmonary system:Pericarditis, pleuritis, pneumonia, shortness of breath

Diagnosis
Common Diagnostic Methods
Diagnosis is based on a combination of clinical symptoms and immunological tests. Doctors typically assess medical history, conduct physical exams, blood tests, and organ function evaluations to confirm the condition and rule out other diseases.
Clinical evaluation:Inquiry into recent symptoms such as rashes, joint pain, fatigue, and examination of skin, joints, heart, and lungs
Immunological tests:
Antinuclear Antibody (ANA):Positive in nearly all SLE patients, but not sufficient alone for diagnosis
Anti-dsDNA:Highly specific and often correlates with disease activity
Anti-Sm:Less common but diagnostically significant
Blood tests:Complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) to assess inflammation
Complement levels:Decreased C3 and C4 levels are common during active disease
Organ function tests:
Kidney function:Urine protein, serum creatinine to detect lupus nephritis
Heart and lung function:Evaluation for complications such as pericarditis and pleuritis

Treatment
Treatment focuses on controlling disease activity, relieving symptoms, and preventing organ damage.
Non-steroidal anti-inflammatory drugs (NSAIDs)
For joint pain, muscle aches, and fever
Antimalarial drugs (e.g., hydroxychloroquine)
Commonly used to manage rashes, arthritis, and fatigue; helps reduce flare-ups
Corticosteroids
Rapidly suppress immune response during acute flares; long-term use requires caution due to side effects
Immunosuppressants (e.g., cyclophosphamide, azathioprine, methotrexate)
For moderate to severe cases to reduce immune system attacks
Biologics (e.g., belimumab)
Targeted therapies for patients unresponsive to conventional treatments
Supportive care
Includes kidney-protective medications, antihypertensives, anticoagulants, and lifestyle adjustments (e.g., avoiding UV exposure, ensuring adequate rest)
Fertility Concerns
Historically, pregnancy was discouraged in lupus patients due to:
Unstable disease:Increased risk of flare-ups during pregnancy;
Medication effects:Some drugs (e.g., cyclophosphamide) may cause early menopause and reduce fertility;
Antibody risks:Certain antibodies (e.g., antiphospholipid syndrome) increase risks of pregnancy complications such as hypertension or preeclampsia; anti-La and anti-Ro antibodies may cause fetal heart block
However, with medical advancements, women with stable lupus (for at least six months) can safely conceive under medical supervision.
Doctors typically coordinate care by adjusting medications, monitoring antibody levels, and working closely with rheumatologists and obstetricians. Many successful cases have been reported, with healthy babies born to mothers with lupus. Additionally, the genetic risk of passing on lupus is relatively low—about 8% to 10%, much lower than commonly assumed.

