Understanding Osteoporosis
Osteoporosis
According to the World Health Organization, osteoporosis is a progressive and systemic disease characterized by decreased bone density and deterioration of bone tissue, leading to increased bone fragility and a significantly higher risk of fractures.
Osteoporosis is very common, particularly affecting postmenopausal women and the elderly. Studies show that about half of women over the age of 65 have osteoporosis. Since the condition often presents no obvious symptoms in its early stages, many patients only become aware of it after experiencing a fracture. Common fracture sites include the hip, spine, and wrist. These fractures can severely impact quality of life and may even increase the risk of mortality.
Causes and Symptoms
What causes osteoporosis?
Bone is a dynamic organ. The body continuously produces new bone tissue while breaking down and replacing old tissue.
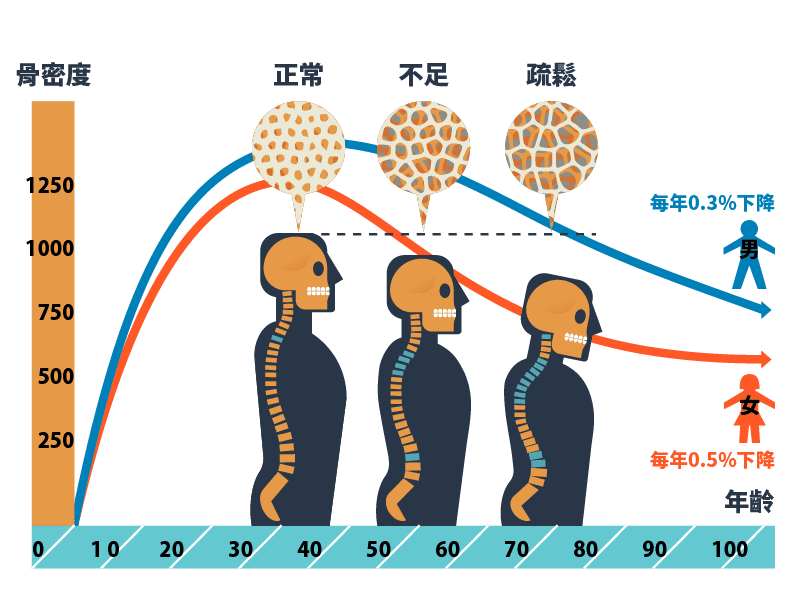
Bone mass increases rapidly during childhood and adolescence, peaks in the 30s, and remains relatively stable during early adulthood. Around the age of 40, bone loss becomes more apparent. In postmenopausal women, declining estrogen levels accelerate bone loss. When bone loss exceeds the normal rate, the risk of developing osteoporosis and fractures increases.
Risk factors include:
-
Age:Older adults
-
Gender:Female
-
Ethnicity:Asian and White people
-
Body type:Low body weight or small frame
-
Family history:Family history of osteoporosis or fractures
Lifestyle-related factors:
-
Long-term insufficient calcium intake, especially in women who diet or have poor eating habits
-
Smoking
-
Excessive alcohol consumption
-
High intake of caffeinated beverages
-
High-salt diet
-
Lack of physical activity
Disease-related factors:
-
Estrogen deficiency in women, such as early menopause (before age 40), premature menopause (ages 40–45), or surgical removal of ovaries
-
Endocrine disorders, such as hyperthyroidism
-
Chronic illnesses, vitamin D deficiency, or history of intestinal surgery
Medication-related factors:
-
Long-term use of corticosteroids
-
Other medications that affect bone metabolism

Common Symptoms of Osteoporosis
Osteoporosis is often called the “silent killer” because it typically has no obvious symptoms in its early stages. As the condition worsens, common symptoms include:
Back or lower back pain: Persistent or chronic pain, often due to vertebral compression fractures
Loss of height:Gradual collapse of spinal bones leading to reduced height
Spinal deformity:May result in a hunched back or abnormal posture, affecting appearance and mobility
Frequent fractures:Even minor falls or pressure can cause fractures, especially in the hip, wrist, and spine
Limited mobility:Fractures may lead to prolonged bed rest or permanent mobility issues

Diagnosis
Since early-stage osteoporosis has no obvious symptoms, regular screening is crucial. High-risk individuals (e.g., women over 65 or those with a family history of fractures) should undergo regular bone density testing. Based on the results, doctors may recommend medication, nutritional supplements, exercise, and lifestyle changes.
Medical history and clinical assessment :Doctors will assess whether the patient has experienced fragility fractures (e.g., fractures from minor falls) and evaluate age, gender, family history, and lifestyle risk factors.
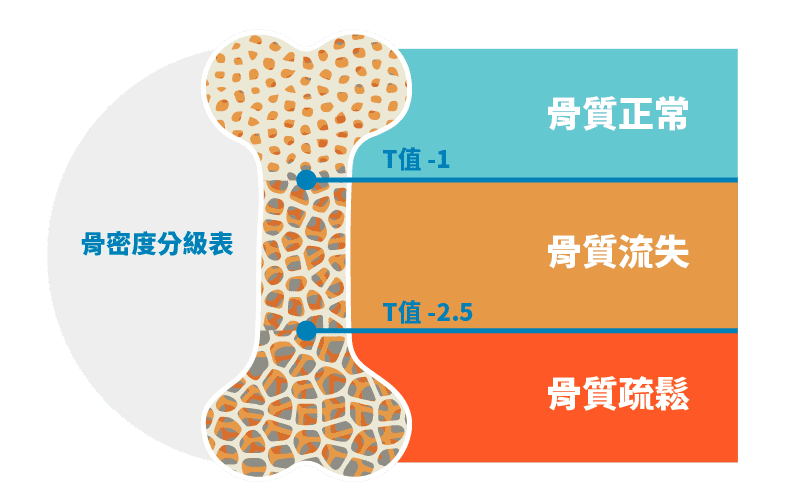
Bone Mineral Density Test (DXA):The most common diagnostic method is dual-energy X-ray absorptiometry (DXA), which uses low-dose X-rays to measure bone density in the lumbar spine and hip. Results are expressed as T-scores:
-
T-score ≥ -1:Normal
-
T-score between -1 and -2.5:Low bone mass (osteopenia)
-
T-score ≤ -2.5:Osteoporosis
-
T-score ≤ -2.5 with fractures:Severe osteoporosis
Fracture Risk Assessment(FRAX®):When bone density is low, doctors use the FRAX® tool to calculate the 10-year probability of fractures based on age, gender, weight, medical history, and other factors. If the risk of hip fracture is ≥3%, or the risk of major osteoporotic fracture is ≥20%, medication is recommended. In Hong Kong, a threshold of ≥9.95% for major osteoporotic fractures is suggested for initiating treatment.
Ultrasound screening:Commonly used on the heel bone; simple and quick, suitable for general screening
CT scan (CT):Provides 3D images of bone structure; less commonly used for routine diagnosis
Blood tests:Used to rule out other conditions affecting bone health (e.g., hyperthyroidism)
Treatment Options
Medication
-
Anti-resorptive agents:Such as bisphosphonates, which slow down bone loss
-
Bone-forming agents:Such as parathyroid hormone analogs (e.g., Teriparatide), which stimulate new bone formation
-
Dual-action agents:Such as Denosumab, which both inhibit bone resorption and promote bone formation
-
Medications are available in oral, injectable, or intravenous forms, with dosing frequencies ranging from daily to biannually.
Nutritional Supplements
-
Calcium:Recommended daily intake for adults is about 1000–1200 mg
-
Vitamin D:Aids calcium absorption and supports bone health; recommended daily intake is 800–1000 IU
-
If dietary intake is insufficient, supplements may be advised by a doctor.
Lifestyle Modifications
-
Engage in regular weight-bearing exercises (e.g., walking, jogging, yoga) to strengthen bones
-
Quit smoking and reduce alcohol consumption
-
Avoid excessive caffeine and high-salt diets
Fracture Prevention and Management
-
Home safety measures:Prevent falls (e.g., use non-slip mats, ensure adequate lighting)
-
Physical therapy:Improve balance and muscle strength to reduce fall risk
-
Regular bone density testing. Monitor treatment effectiveness

