Understanding Thyroid Diseases
Thyroid Diseases
Thyroid diseases are very common in Hong Kong, ranking as the second most prevalent endocrine disorder after diabetes. Women aged 30 to 50 are considered a high-risk group. Common thyroid conditions include hyperthyroidism, hypothyroidism, benign thyroid nodules, and thyroid cancer, primarily related to functional abnormalities or structural changes of the thyroid gland.
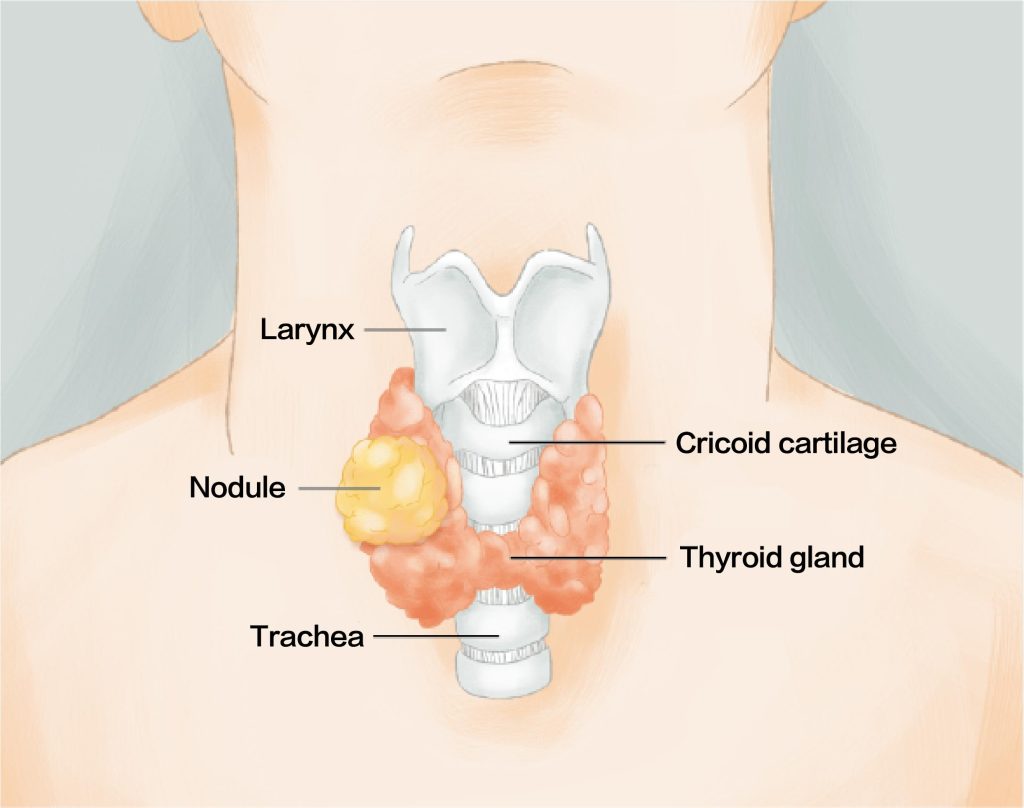
What Is the Thyroid?
The thyroid is a vital organ in the endocrine system, shaped like a butterfly with wings spread, located in the lower front part of the neck. It consists of a left and right lobe and secretes thyroid hormones that regulate metabolism, heart function, and body temperature. These hormones are closely linked to energy levels, growth and development, and the functioning of various organs.
Causes and Symptoms
What Causes Thyroid Diseases?
Thyroid disorders result from a combination of immune, genetic, environmental, and lifestyle factors. Major causes include:
Autoimmune diseases:Hashimoto’s thyroiditis (causing hypothyroidism) and Graves’ disease (causing hyperthyroidism), where the immune system mistakenly attacks thyroid tissue, affecting hormone production.
Iodine imbalance:Iodine is essential for thyroid hormone synthesis. Deficiency can lead to hypothyroidism, while excess may trigger hyperthyroidism or hypothyroidism.
Medications:Drugs like lithium and amiodarone (used for arrhythmias) may suppress thyroid function.
Surgery or radiation therapy:Thyroid removal or neck radiation can damage the gland and cause hypothyroidism.
Genetic and environmental factors:Family history, stress, diet, and viral infections may increase risk.
Nodules or tumors:These may alter gland structure and disrupt function.

Common Symptoms of Thyroid Diseases
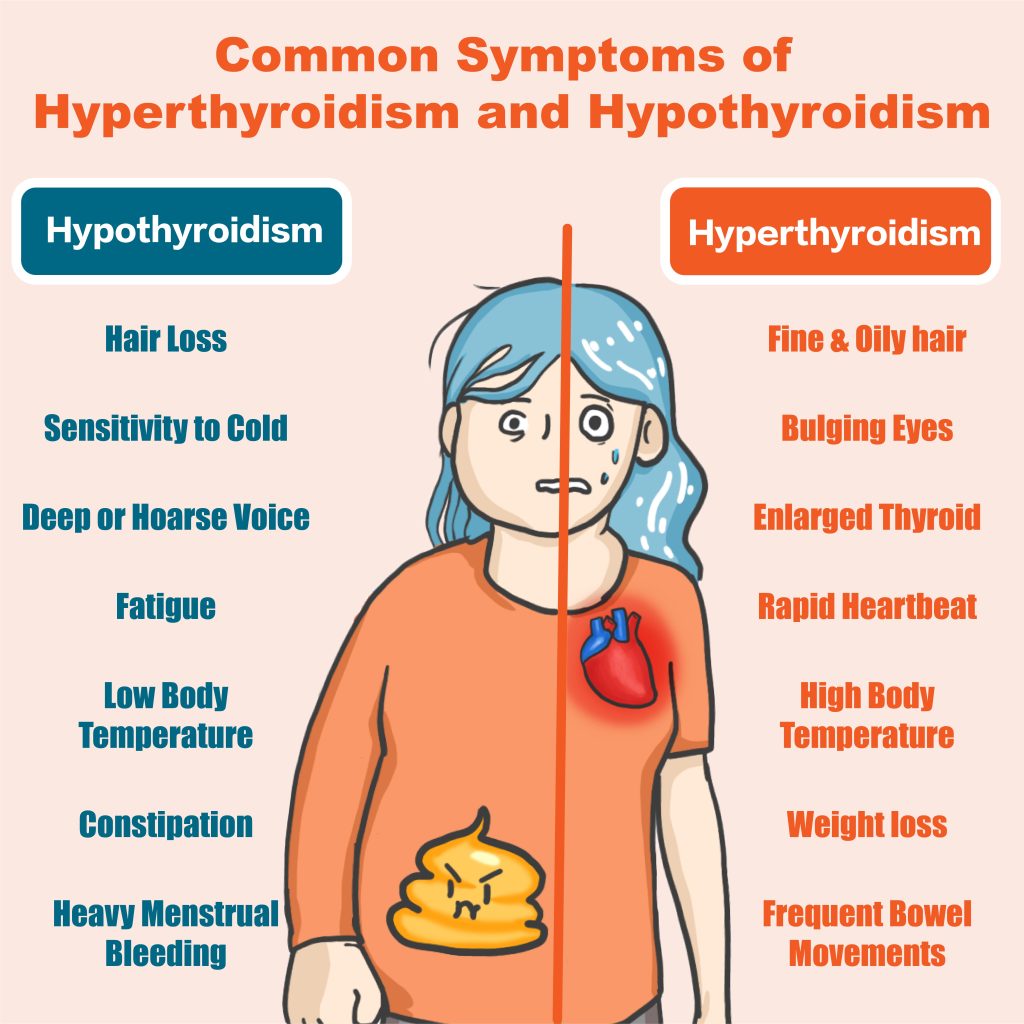
Hyperthyroidism (Overactive Thyroid)
Rapid heartbeat, palpitations
Tremors, anxiety, insomnia
Weight loss (despite normal or increased appetite)
Heat intolerance, excessive sweating, elevated body temperature
Increased bowel movements, diarrhea
Bulging eyes (common in Graves’ disease)
Hypothyroidism (Underactive Thyroid)
Slowed metabolism, fatigue, poor concentration
Weight gain, cold intolerance
Dry skin, reduced sweating
Swelling, hoarse voice
Memory decline, depression
Thyroid Nodules or Tumors
Often asymptomatic in early stages
Enlarged nodules may press on the trachea or esophagus, causing breathing or swallowing difficulties
Palpable neck lumps
Other Common Signs
Neck swelling or pain
Hoarseness (due to pressure on vocal cord nerves)
Irregular menstrual cycles or abnormal flow
Mood changes: irritability in hyperthyroidism, depression in hypothyroidism
Diagnostic Methods
Diagnosis typically begins with blood tests to assess function, followed by ultrasound to examine structure. Fine needle aspiration or nuclear scans may be used when necessary. Early medical evaluation is recommended for neck lumps or abnormal symptoms.
Blood tests:Measure TSH, T4, and T3 levels to determine hyper- or hypothyroidism.
Thyroid ultrasound:Evaluates size, shape, and structure; detects nodules, cysts, or masses.
Fine Needle Aspiration (FNA):Extracts cells from nodules to determine if tumors are benign or malignant.
Nuclear scan:Uses radioactive iodine or other tracers to assess function and structure, commonly used for hyperthyroidism.
Laryngoscopy:Examines vocal cord movement, especially if tumor compression is suspected.
Physical exam and history:Doctors palpate neck lumps and inquire about symptoms like palpitations, weight changes, or swallowing issues.

Treatment Options
Treatment usually starts with medication to control hormone levels, followed by surgery or radiation depending on structural issues or tumor type. Long-term follow-up is often required, and some patients may need lifelong medication to maintain hormonal balance.
Antithyroid drugs
Used for hyperthyroidism to suppress hormone production. Treatment typically lasts 18–24 months, but relapse may occur after stopping.
Radioactive iodine therapy
Taken orally, it travels through the bloodstream to the thyroid, destroying part or all of the gland. Patients may need lifelong hormone replacement afterward.
Surgical removal
Recommended for large goiters compressing the airway or esophagus, suspected cancer, or severe eye symptoms. Post-surgery hormone supplementation is usually necessary.
Thyroid hormone replacement
Used for hypothyroidism, involving synthetic hormones (e.g., levothyroxine) to maintain normal metabolism.
Chemotherapy or radiation therapy
Primarily for thyroid cancer, depending on tumor type and stage.

