Cervical Screening
Cervical Screening
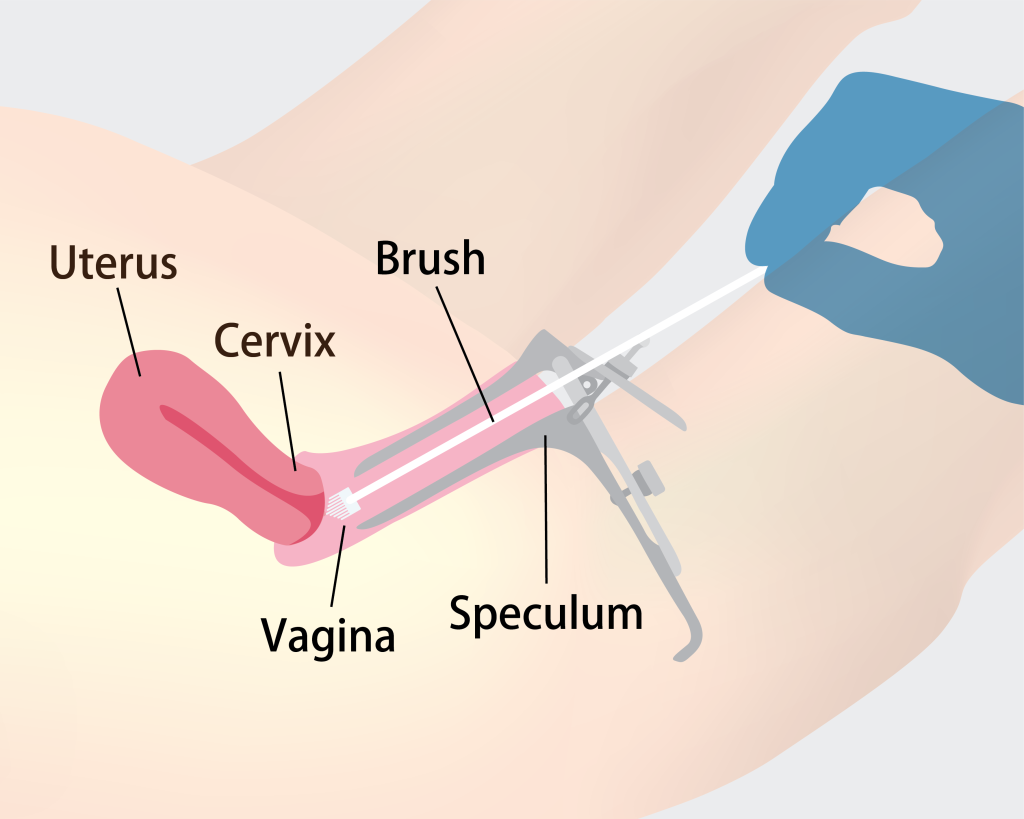
Cervical screening is a quick and simple test used to detect early abnormal changes in the cells of the cervix.
The cervix is located at the lower part of the uterus, connecting the uterus to the vagina. During screening, a doctor or nurse gently inserts a speculum into the vagina to clearly view the cervix. A special brush is then used to collect cell samples from the surface of the cervix, which are sent to a laboratory for testing.
Common Cervical Screening Methods
Pap Smear (Cervical Cytology Test)
The Pap smear is a simple and safe gynecological test used to detect abnormal changes in cervical cells. Regular screening can reduce the risk of cervical cancer by over 90%.
The test involves collecting cervical secretions using medical instruments to check for the presence of high-risk human papillomavirus (HPV), which can lead to cervical cancer. The procedure takes only a few minutes and is generally safe, with minimal discomfort.
It’s important to note that abnormal cells do not necessarily mean cancer. If abnormalities are found, doctors usually recommend further tests, such as a colposcopy, to determine the nature of the changes.

Human Papillomavirus (HPV) Test
The HPV test detects whether a woman is infected with high-risk types of human papillomavirus. Persistent infection with high-risk HPV is the main cause of cervical cancer and can lead to abnormal cell changes or precancerous lesions.
HPV testing effectively identifies high-risk infections and complements the Pap smear, making it an important tool in cervical cancer prevention.
Recommended Screening Groups and Frequency
HPV is the primary cause of cervical cancer and is mainly transmitted through sexual contact. Women aged 25 and above who are sexually active are advised to undergo regular cervical screening, which can prevent over 90% of cervical cancer cases.
Recommended Screening Frequency
Women aged 25–29:
Undergo Pap smear screening annually for two consecutive years. If results are normal, continue screening every three years.
Women aged 30–64:
If two consecutive Pap smear results are normal, continue screening every three years; or
Undergo HPV testing every five years; or
Undergo co-testing (HPV + Pap smear) every five years.
Women aged 65 and above:
If screening results have been consistently normal over the past ten years, screening may be discontinued. However, women who have never been screened are still advised to undergo testing.
Special Circumstances Requiring Prompt Screening:
Unusual vaginal bleeding (e.g., between periods or after intercourse)
Abnormal vaginal discharge with odor
Pain during intercourse
Vaginal bleeding after menopause
Persistent or unexplained pelvic pain
